October 4, 2023
It takes a village
Exploring potential synergies between B- and T-cell HIV vaccine strategies is a priority for the field given results from recent trials.
Kristen Kresge Abboud
There is a well-known children’s book by Shel Silverstein about a circle that is missing a pie-shaped slice, and so it sets out on an adventure to find its missing piece. Along the way it comes across many shapes that don’t quite fit. Then, at long last, it finds the perfect triangle to make it complete.
For HIV vaccine researchers, the missing piece they’ve been searching for is a way to induce so-called broadly neutralizing antibodies (bnAbs) against the virus that are effective at blocking many of the diverse HIV variants that are in circulation worldwide. This is a huge challenge because formation of these bnAbs is disfavored in many ways—they develop only rarely in people living with HIV, and only after several years of chronic infection with a constantly mutating virus.
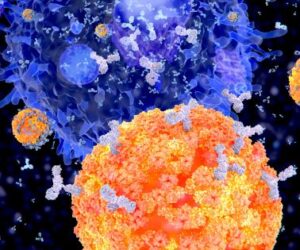
Plasma cells (B-cells) segregate specific antibodies to mark and subsequently destroy viruses.
These antibodies have also proven difficult to induce through vaccination. Researchers are still investigating whether multi-step immunization strategies can train the immune system to produce these highly mutated bnAbs, but many challenges remain. “We’re trying to make a series of rare events common,” says Barton Haynes, Director of the Human Vaccine Institute at Duke University. Which is why, after four decades of research, the search for the missing piece continues.
The good news is that evidence suggests that scientists are headed in the right direction. Results from the Antibody Mediated Prevention (AMP) trials showed that passive administration of bnAbs with sufficient specificity can protect against HIV infection if they are present at high enough concentrations. These results provide an important proof of concept for the role of bnAbs in protecting against HIV. But, at the same time, the AMP trials also showed just how difficult it may be to induce protective immunity through bnAbs alone, according to Shane Crotty, Chief Scientific Officer of the Center for Infectious Disease and Vaccine Research at the La Jolla Institute for Immunology.
Antibodies, even those that are broadly neutralizing, may need a little help from their friends, which, in this case, are T-cells. Researchers are increasingly interested in harnessing the power of cellular immunity to try to augment both innate and adaptive immune responses against the virus and lower the bar for protection by bnAbs.
Data from preclinical studies suggest that combining B- and T-cell vaccines can be more effective than either strategy alone. “Protection is a complex phenomenon,” says Paolo Lusso, Chief of the Viral Pathogenesis section at the U.S. National Institutes of Health (NIH). “One plus one is not always two.”
Lusso argues that working on B- and T-cell vaccines in isolation isn’t ideal. He suggests a more holistic approach instead, an idea the field seemed to coalesce around at a two-day virtual symposium in August convened by the U.S. National Institute of Allergy and Infectious Diseases (NIAID) to explore potential synergies between B- and T-cell focused HIV vaccine strategies. Leading immunologists and HIV vaccine researchers reviewed data on the B- and T-cell vaccine candidates in development and identified opportunities to combine them to optimize immunity and accelerate the development of a preventive HIV vaccine.
The power of synergy
B and T cells work together in multiple ways. One that is attracting interest from HIV vaccine researchers comes from the results of a preclinical study conducted by Bali Pulendran, a professor of microbiology and immunology at Stanford University, and colleagues. This study showed that an HIV protein vaccine candidate that induced neutralizing antibodies against harder to neutralize so-called tier-2 viruses combined with a potent T-cell vaccine provided better protection against a mucosally administered challenge virus (a hybrid of simian immunodeficiency virus/HIV hybrid known as SHIV) in rhesus macaques.
Perhaps even more importantly, the combination antibody/T-cell vaccine was protective even at lower, sub-optimal titers of neutralizing antibody. These results suggest that adding a T-cell vaccine helped lower the threshold required for protection by neutralizing antibodies. The combined B- and T-cell vaccines tested in this study also provided more durable protection, which is another critical factor for any future HIV vaccine.
Researchers hypothesize that the presence of HIV-specific CD8+ T cells induced by the vaccine in vaginal tissues may help transduce B-cells into tissues, where they can secrete antibodies, in addition to activating local innate immune responses, all of which work together to boost protection. Pulendran summarized these findings at the workshop and described them as a clear example of how the complex yet critical interactions between innate and adaptive immune responses will be required to achieve the goal of a highly effective preventive HIV vaccine.
Now, the goal is replicating these findings and expanding upon them. Rama Amara and colleagues at the Emory Vaccine Center have already begun confirmatory studies to evaluate several different prime-boost combinations of viral vectored T-cell vaccines. The goal is to see which of them in combination with a native-like HIV Envelope trimer immunogen will provide the best protection.
There was extensive discussion at the workshop on the best vectors for inducing CD8+ T-cell responses in mucosal tissues. Several participants, including Robert Seder, acting chief of the Vaccine Immunology Program at the Vaccine Research Center at NIAID, argued in favor of live, replicating viral vectors for their ability to induce long-lived T-cell responses at multiple sites.
Among the replicating vectors, the cytomegalovirus (CMV) vaccine vector developed by researchers at Oregon Health & Sciences University (OHSU) seems to be one of, if not the, most promising, at least based on preclinical data. Several studies over the past two decades have shown that their rhesus CMV-based SIV vaccine can reproducibly eliminate infection in between 50% to 60% of rhesus macaques exposed to repeated, mucosally administered SIV challenges.
Further work by Louis Picker and Klaus Fruh at OHSU helped identify the mechanism of this viral control/elimination. Thanks to a serendipitous deletion of certain genes in the wildtype virus, the rhesus CMV vaccine vector induces an unusual type of CD8+ T cell. Vaccine antigens are presented to T cells via a series of genes known as the major histocompatibility complex or MHC. The rhesus CMV vector induces CD8+ T cells that are restricted by an MHC class Ib molecule known as human leukocyte antigen (HLA)-E, and this unconventional signaling pathway is associated with the efficacy of the vaccine. Additional studies show that a cytokine known as interleukin (IL)-15 — a known regulator of CD8+T-cell function — also correlates with the efficacy of the rhesus CMV vaccine vector.
Researchers are now eager to find out if eliciting the same MHC-E restricted CD8+ T-cell responses in humans will yield similar results to those from preclinical studies. Vir Biotechnology is currently testing a human CMV vector in in humans, according to a presentation at the symposium by Ann Arvin, Senior Vice President of Vir.
In the meantime, Fruh is collaborating with Dennis Burton, Chair of the Immunology and Microbiology Departments at Scripps Research and scientific director of IAVI’s Neutralizing Antibody Center, to test the rhesus CMV vector-based T-cell vaccine in combination with sub-optimal doses of passively administered bnAbs to see if there is any synergy between these two approaches. According to Jonah Sacha, a professor at OHSU, the CMV vector induces very little, if any, antibody response and therefore combining it with bnAbs could balance the strengths and weaknesses of the two approaches.
This study and others like it will help researchers understand the synergies between different components of the immune response. Scientists at the symposium argued for more preclinical studies that can compare different viral vectors, immunogens, adjuvants, and routes of administration to help identify the best T-cell vaccine candidates to test in combination with passively administered bnAbs, and eventually with vaccine regimens that can induce bnAbs, in human clinical trials.
One challenge of this work will be measuring and characterizing the immune responses induced by these combination regimens. For antibodies, researchers now know what concentration of antibody is required for protection. However, on the T-cell side, there isn’t as clear a marker of success. Apart from the induction of MHC-E restricted CD8+ T cells, researchers don’t know precisely what constitutes an effective cellular immune response against the virus.
And these responses are also difficult to measure in tissues. Sampling is more invasive, and analysis of the samples is much more technically difficult. Yet it will likely be critical to understand both T- and B-cell responses in blood and tissues to fully determine how well these vaccine strategies are working.
While there are still many obstacles to developing an HIV vaccine, this symposium illustrated once again that researchers are fully committed to overcoming these obstacles and are aligned on the importance of looking for and optimizing the synergies between humoral and cellular immunity to facilitate progress.”